Decoding Covid-19
Seven human coronaviruses in seven graphics
By the end of the day, there will be probably 550,000 Covid-19 cases , resulting in almost 24,000 fatalities worldwide. After its discovery last December, in Wuhan, China, the virus started to spread around the world, causing panic. The Antarctic is, as yet, the only continent where there are no confirmed cases.
There are seven types of coronaviruses that are contagious for humans. Four types (NL63, 229E, OC43 and HKU1) are responsible for 15 to 30% of the world’s common cold cases every year and are considered endemic.
Two other types are considered epidemic: the Sars outbreak, which affected 26 countries and first infected humans in the Guangdong province of southern China in 2002, and Mers, which was first reported in 2012 and is prevalent in the Middle East.
The seventh coronavirus is Sars-Cov-2, the novel coronavirus that causes Covid-19, whose origins are unconfirmed at the moment.
In an interview with the South China Morning Post, microbiologist Eugenia Corrales-Aguilar, who has a PhD in virology from Humboldt University in Berlin, outlined the facts on Covid-19.
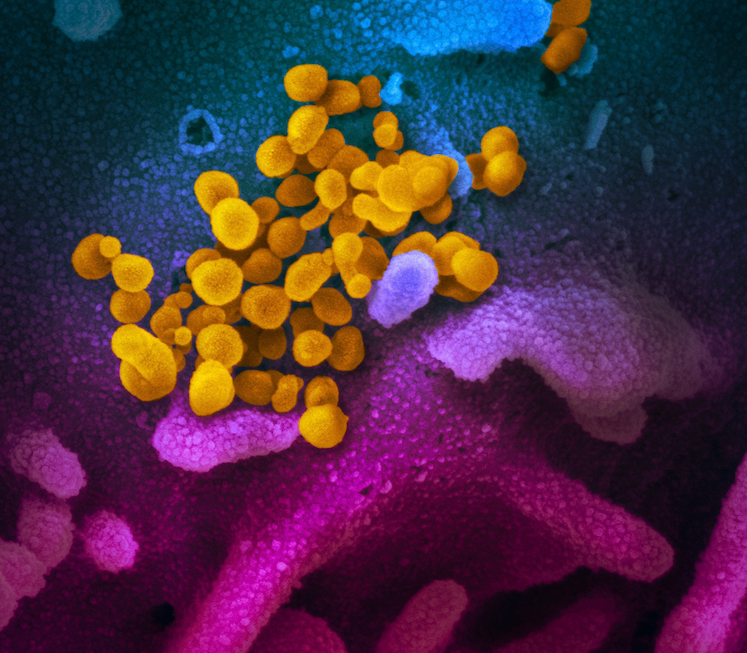
The data obtained so far shows that Sars-Cov-2, ranges from mild-medium to severe. From a molecular point of view, coronaviruses have some variations in their genetic sequence as well as the cellular receptor they use.
In this case, Sars-Cov-2 uses ACE2 as receptors, which are mostly found in the respiratory tract. The virus infects the target cells causing damage. The resulting inflammatory and immune response can cause pneumonia to develop in most severe cases. The impact depends on the individual and how their body reacts.
How does Covid-19 spread?
At the moment, we know that the virus is transmitted through contaminated droplets. Droplets of saliva or mucus carrying the respiratory virus can travel one to three metres through coughing or sneezing. The virus needs to fully enter the respiratory tract for infection to happen, but that\’s why the risk of infection can be reduced by avoiding close contact with sick people. Washing your hands thoroughly greatly reduces the risk of infection.
There are reports that infection is possible through faeces and recirculated air ventilation systems and air conditioners. But this has not been systematically studied, so it is hard to say with 100 per cent certainty.
How deadly is the new coronavirus compared to Sars, Mers and the four coronaviruses that cause the common cold?
We cannot determine this for certain yet as the apparent mortality rate is likely to be overestimated at the start of an outbreak, because a lot of mild cases are missed. Also, with Covid-19, some people can be asymptomatic – meaning the virus is not always detected and therefore not recorded.
The mortality rate for influenza is 0.1 per cent, but since Covid-19 is so new it remains to be seen just how many cases will turn out to be fatal.
It is commonly cited that in a given year with no complications, influenza kills 500,000 people. Compared to the four respiratory coronaviruses, the mortality rate for Sars-Cov-2 is higher. Although compared to Sars (9.6 per cent) and Mers (34.4 per cent), Covid-19 shows a low mortality rate but with a wider spread, making the total number of deaths larger.
Among those infected, how many people will develop a more severe infection?
According to current data, the percentage of people who develop a severe infection is 15 per cent and 5 per cent are critically ill– a great stress on health care systems.
How long will it take before a vaccine for the new coronavirus is publicly available? How long did it take for Sars and Mers?
After the disappearance of Sars, all financial aid and investigation programmes regarding the creation of a vaccine were cut. The Mers vaccine is a work in progress, with the syndrome still affecting people. For Sars-Cov-2, an optimistic estimate would be one to two years because it needs to go through clinical trials after it is developed in the lab and, if effective, then produced on a large scale.
Natural immunity after coronavirus infection decreases over time, which is why reinfection from the four respiratory coronaviruses takes place, making it very difficult to create a vaccine that raises a lasting protective immune response.
What could happen is that a developed vaccine might not be able to prevent infection but might be able to reduce the severity – this is the case with influenza vaccines, which should be administered once a year. Even so, this is a process that takes time.
Therefore, hygiene measures like thorough handwashing, sensible coughing and sneezing protocol and maintaining social distance are, for now, the best ways to prevent the spread of the virus.
Can a patient become infected again after successfully recovering?
If time elapses and natural immunity is no longer present or it is not effective any more, yes, they can. In the case of the four respiratory coronaviruses, cases of reinfections are observed after eight to 12 months. It has not been determined for Sars-Cov-2 yet due to its novelty.
Also, we don’t use the term \”carrier\”, as is the case of HIV or some hepatitis viruses, because Covid-19 is considered a \”hit-and-run\” virus. This means that when a person gets infected, the immune system is activated and the infection is \”cleaned\”.
Can summer, or warmer temperatures for that matter, help eradicate the virus?
For some respiratory viruses this does happen. Not just because of the temperature, but also thanks to the humidity and changes in social patterns of human beings. In this case, it is still premature to say if this is going to happen. Let\’s hope so…
Full article with graphics available here courtesy of South China Morning Post and Pablo Robles
You might also like
For relevant updates on Emergency Services news and events, subscribe to EmergencyServices.ie